Can You Have Anxiety and Depression at the Same Time? Understanding the Connection
Anxiety and depression are often talked about as separate experiences. Anxiety is described as too much… too many thoughts, too much worry, too much anticipation. Depression is often framed as not enough… not enough energy, not enough motivation, not enough feeling.
But for many people, anxiety and depression don’t take turns. They coexist.
You can feel deeply exhausted and still unable to relax.
You can feel hopeless and still worry constantly.
You can want to disappear and feel on edge all the time.
If you’ve ever thought, “I don’t even know what I’m dealing with anymore, am I anxious or depressed?” …this is a common question we hear at Better Minds Counseling & Services. And no, it doesn’t mean you’re “too much” or “too complicated.”
Continue on to learn the breakdown of how anxiety and depression can coexist, what symptoms look like when they overlap, how this shows up in real life, and five ways a therapist can help you untangle what’s going on.
You don’t have to figure out alone if you are more anxious or more depressed…. we have therapists here to help.
Why Anxiety and Depression Often Coexist
Anxiety and depression share many of the same biological, emotional, and environmental roots. Both impact how your nervous system functions, how your brain processes threat and safety, and how your body responds to stress.
Anxiety often keeps your nervous system in a state of hyperarousal; always scanning, anticipating, bracing for what could go wrong. Over time, living in that constant state of tension is exhausting. Depression can develop as the body’s response to prolonged overwhelm: shutting down, conserving energy, pulling inward.
In simple terms:
Anxiety burns you out
Depression moves in once you’re depleted
They’re not opposites. They’re connected.
Common Symptoms When Anxiety and Depression Overlap
When anxiety and depression coexist, symptoms don’t always fit neatly into diagnostic boxes. Instead, they blend together in ways that can feel confusing or even invalidating.
Emotional Symptoms
Feeling constantly overwhelmed and emotionally numb
Persistent worry mixed with hopelessness
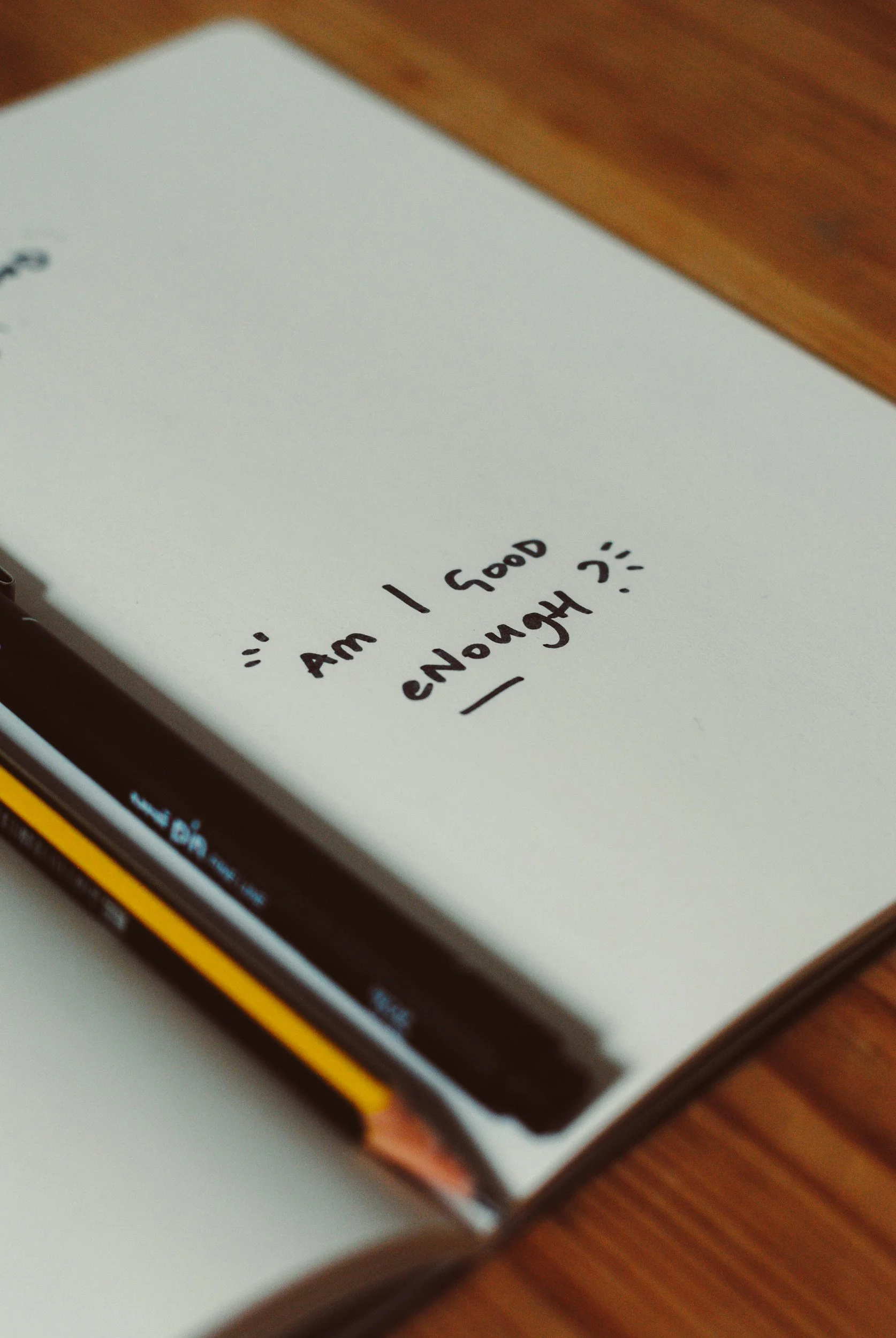
Guilt about not doing “enough,” paired with fear of doing things wrong
Irritability that feels out of proportion, followed by shame
A sense of heaviness while your mind won’t slow down
Cognitive (Thought-Based) Symptoms
Racing thoughts that loop around self-criticism
“What if” thinking mixed with “what’s the point” thinking
Difficulty concentrating or making decisions
Catastrophizing future outcomes while feeling stuck in the present
Overthinking conversations, mistakes, and imagined failures
Physical Symptoms
Chronic fatigue even after sleeping
Trouble falling or staying asleep due to racing thoughts
Muscle tension, headaches, or jaw clenching
Digestive issues or appetite changes
A heavy or restless feeling in the body, sometimes both at once
Behavioral Symptoms
Withdrawing socially but feeling lonely
Cancelling plans out of exhaustion and anxiety
Procrastination paired with harsh self-judgment
Difficulty starting tasks, even ones you care about
Using distractions (scrolling, working nonstop, substances) to escape how you feel
You work harder and harder… and it doesn’t get better.
What This Can Look Like in Real Life
Example 1: The High-Functioning Struggle
You go to work. You meet deadlines. You show up for others. From the outside, you seem “fine.”
Inside, you wake up already anxious. Your chest feels tight before the day even starts. You replay conversations from yesterday and worry about ones that haven’t happened yet. By evening, you’re completely drained, but instead of relaxing, you feel flat and disconnected.
You tell yourself, “Other people have it worse. I should be grateful.” But you still feel miserable.
This is a common anxiety–depression overlap: functioning on the outside, suffering quietly on the inside.
Example 2: Avoidance Fueled by Fear and Hopelessness
You avoid emails, phone calls, or social plans. Anxiety tells you something will go wrong. Depression tells you it won’t matter anyway.
So you stay stuck.
Each avoided task increases anxiety. Each day of avoidance deepens shame and low mood. The cycle reinforces itself, leaving you feeling trapped and frustrated with yourself.
Example 3: Emotional Whiplash
Some days you feel wired—restless, edgy, unable to sit still. Other days you feel heavy, slow, and disconnected.
You might think, “Why can’t I just pick one?”
But this fluctuation is common when anxiety and depression coexist. Your nervous system is constantly swinging between overdrive and shutdown.
Why It’s Hard to Talk About
Many people hesitate to seek help because they don’t know how to explain what they’re feeling. You might worry:
“I don’t feel bad enough”
“I should be able to handle this”
“I don’t want to be dramatic”
“What if I’m just lazy or broken?”
Anxiety and depression together often create self-doubt about whether your pain is valid. Therapy isn’t about deciding if you’re “sick enough.” It’s about understanding what your system is going through and helping you feel more like yourself again.
When self-doubt creeps in, it is hard to move past being hypercritical of yourself.
How a Therapist Can Help (5 Key Ways)
1. Helping You Make Sense of What You’re Experiencing
One of the biggest reliefs therapy offers is clarity. A therapist helps you untangle which symptoms are rooted in anxiety, which are connected to depression, and how they interact.
Instead of feeling like a mess of symptoms, you start to understand patterns:
What triggers your anxiety
What deepens your low mood
How stress, relationships, or burnout play a role
Understanding reduces shame and shame is often what keeps people stuck.
2. Regulating Your Nervous System
When anxiety and depression coexist, your nervous system is often dysregulated. Therapy helps you learn how to gently bring your body back into balance.
This might include:
Grounding techniques
Breathing practices
Somatic awareness (noticing how emotions live in your body)
Learning when to slow down vs. when to activate
The goal isn’t to “calm down” all the time; it’s to feel safer and more stable in your body.
3. Challenging Unhelpful Thought Patterns (Without Invalidating You)
Anxiety and depression both distort thinking, but in different ways. Anxiety exaggerates threat. Depression minimizes hope.
A therapist helps you notice these patterns without telling you to “just think positive.” Together, you work on creating more balanced, compassionate internal dialogue that feels believable, not forced.
4. Rebuilding Energy, Motivation, and Self-Trust
When you’re anxious and depressed, even small tasks can feel overwhelming. Therapy helps you:
Set realistic expectations
Break tasks into manageable steps
Reduce all-or-nothing thinking
Reconnect with values and meaning
Over time, this rebuilds confidence and self-trust; two things anxiety and depression often erode.
5. Offering a Space Where You Don’t Have to Perform
Many people feel pressure to appear okay. Therapy is a space where you don’t have to explain away your feelings or minimize your pain.
You get to show up exactly as you are:
Tired
Confused
Irritable
Tearful
Numb
Being seen and supported without judgment is not a small thing; it’s often a turning point.
You Don’t Have to Untangle This Alone
Anxiety and depression coexisting doesn’t mean you’re failing at coping. It means your system has been under strain for a long time.
With the right support, it is possible to:
Feel less overwhelmed
Regain energy and motivation
Quiet the constant mental noise
Feel more present in your life and relationships
Therapy isn’t about fixing you. It’s about helping you understand yourself, care for your nervous system, and move toward a life that feels more manageable and more yours.
If any part of this resonated, that’s worth paying attention to. Support exists, and you don’t have to wait until things get worse to reach for it. Reach out today to schedule a free intro meeting with a Better Minds therapist.